The body hosts many microorganisms. These include bacteria, viruses, and fungi. Normally, they coexist in balance. But changes in environment or immunity disrupt that harmony. When good bacteria decrease, yeast grows unchecked. The most common culprit is Candida albicans. It thrives in moist, warm environments. Vaginal areas, the mouth, and skin folds are often affected. Disruption allows overgrowth and irritation to begin quietly.
Hormonal changes often trigger fungal overgrowth in otherwise healthy individuals
Fluctuating hormones influence yeast development. During pregnancy, estrogen levels increase sharply. This alters pH balance and encourages fungal growth. The same can happen during ovulation or with oral contraceptive use. Menstrual cycles may also shift microbial activity. The body’s defense weakens under these shifts. Even without external triggers, internal changes allow yeast to thrive.
Antibiotics reduce protective bacteria, creating space for opportunistic fungi to multiply
Antibiotic use is a frequent cause. These medications kill both harmful and helpful bacteria. Without bacterial competition, yeast expands rapidly. A course of antibiotics, even for a few days, can tip the balance. Vaginal yeast infections often follow antibiotic therapy. The risk increases with longer treatment or broad-spectrum drugs. Restoring microbial balance afterward takes time and attention.
Warm, moist environments support colonization, especially in areas with limited airflow
Yeast favors warmth and moisture. Tight clothing, especially synthetic underwear, creates ideal conditions. Sweat and heat build in enclosed areas. The skin cannot breathe properly. Prolonged exposure to these environments increases risk. Commonly affected regions include underarms, under breasts, groin, and between toes. Daily hygiene helps, but material choice and ventilation matter more than expected.
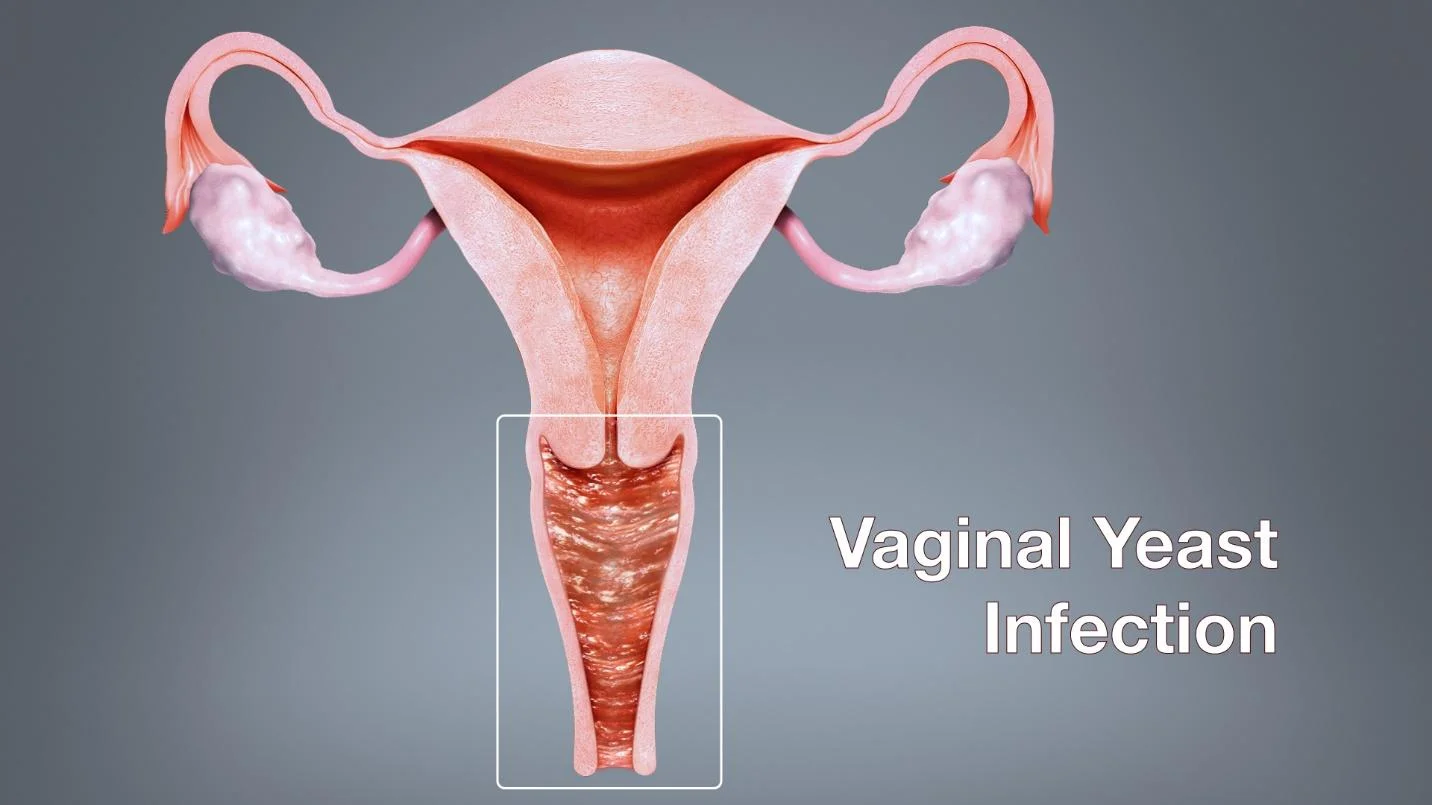
Symptoms often include redness, itching, swelling, and thick white discharge
The signs can vary, but discomfort is consistent. Itching and burning usually appear first. Infections on the skin show redness and small bumps. Vaginal yeast infections produce thick, white discharge resembling cottage cheese. Pain during urination or intercourse may follow. Oral thrush appears as white patches inside the mouth. These symptoms build gradually and may worsen without treatment.
Oral thrush can develop from inhalers, dentures, or a compromised immune response
Not all yeast infections are genital. Oral thrush affects the tongue, cheeks, and roof of the mouth. Inhaled corticosteroids are a common cause, especially without mouth rinsing afterward. Ill-fitting dentures can trap moisture, feeding yeast. Weakened immunity from illness or medication also plays a role. Elderly patients and infants are especially vulnerable. It can become painful or affect eating if untreated.
Diagnosis usually involves visual inspection or microscopic examination of skin or discharge samples
Doctors often recognize infections visually. In ambiguous cases, they examine samples under a microscope. Vaginal swabs, skin scrapings, or oral smears provide confirmation. Cultures may be needed for recurrent cases. These identify the specific yeast strain. That information helps tailor treatment. Not all fungi respond to the same medications. Accurate diagnosis prevents repeated or ineffective therapies.
Topical antifungal creams are effective for many surface infections with minimal side effects
Mild infections respond well to creams. Clotrimazole, miconazole, or terbinafine are common options. These reduce fungal presence and soothe inflammation. Over-the-counter products are widely available. Application continues for several days, even after symptoms improve. This ensures full eradication. Some areas, like under nails or thickened skin, may need stronger treatment. Surface-level remedies work best when used early.
Oral antifungals are prescribed for deeper infections or when topical agents fail
Severe cases may need pills. Fluconazole and itraconazole treat systemic or stubborn infections. These drugs circulate in the bloodstream, targeting fungi throughout the body. They’re used when creams don’t penetrate deeply enough. Liver function must be monitored during treatment. Side effects may include nausea, rash, or rare allergic reactions. Doctors weigh benefits and risks based on history and severity.
Probiotics may help prevent recurrence by restoring beneficial bacteria to mucosal surfaces
After treatment, relapse is possible. Probiotics aim to restore microbial balance. Yogurt with live cultures or supplements may support this. They repopulate areas where good bacteria were lost. Some formulations are vaginal, others oral. Their role remains debated, but anecdotal success is common. Diet, hydration, and hygiene also affect recurrence. Habits after healing influence whether infections return.
Source: Gynecology in Dubai / Gynecology in Abu Dhabi